Implementing three policy recommendations, with short-term and longer-term steps, would increase access to home- and community-based services, reduce institutional bias in the Medicaid program, and create a stronger caregiving workforce, according to a new report from research and advisory firm ATI Advisory.
ATI CEO Anne Tumlinson suggested not only increasing that federal matching rate for Medicaid-funded home- and community-based services, but making it permanent and potentially enhancing it. Doing so, she said, lays out for states a longer-term set of commitments not just to maintain spending levels, but also to implement a long-term workforce plan for developing the direct care workforce, increasing the number of people served through 1915(c) waivers, and ensuring a balance across populations serviced by these dollars.
The blueprint of key policy proposals from ATI, with support from the Robert Wood Johnson Foundation, builds on a rescue package recommendation before Congress that would provide a one-year increase in the federal contribution to Medicaid-funded home- and community-based services such as those provided by some assisted living operators through Medicaid waivers. The blueprint also proposes reforms to Medicaid long-term services and supports to increase access to services and create better caregiving jobs.
Tumlinson said she is “surprisingly hopeful” that the policy recommendations will “move the needle” on Medicaid reform.
“This is a hard, really hard thing to do, because we have so much ground to make up,” she told McKnight’s Senior Living. “For a benefit to be meaningful, people who are performing these services in that benefit have to be well-compensated or the benefit itself is not going to mean anything. We have to have access to a good supply of workers who are well-compensated; we’ve got to be able to expand the numbers of people who get those services — we don’t have that today.”
Tumlinson said the proposal is not an “overnight solution,” but that “if there’s ever a year this could get done, this is it.”
Predictable funding
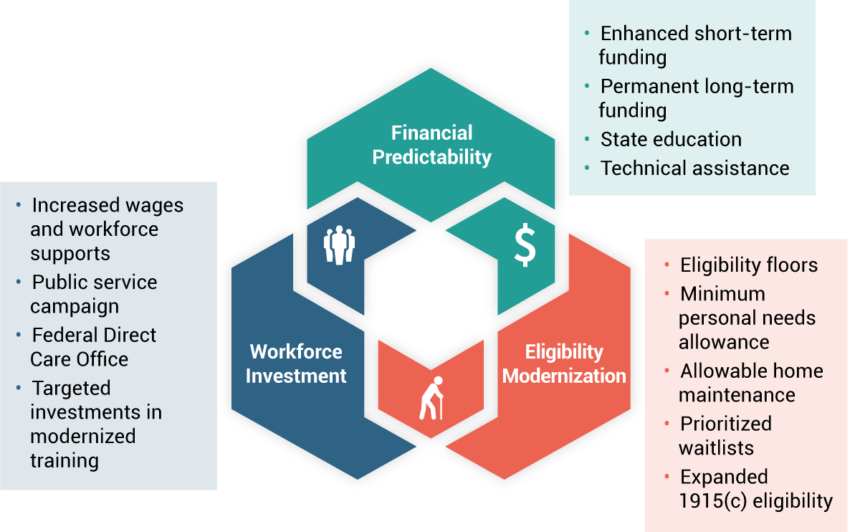
One recommendation from the blueprint is to increase access to HCBS through financial relief and predictability for states.
Medicaid accounts for 29% of total state spending across all funding sources, and LTSS make up a substantial portion of that spending. “This creates financial pressures, resulting in cuts to the Medicaid program during times of budget pressure, and reluctance to provide or expand services that are optional, such as HCBS LTSS,” according to the report.
Immediate suggestions on ways to accomplish the recommendation include policy and financing approaches to “increase access to HCBS by increasing funding and alleviating immediate state financial concerns.” Those can include an enhanced federal match and state education on HCBS financial controls.
Longer-term ways to meet the recommendation include financing reform that federalizes some portion of LTSS, or creation of a shared risk model between states and the federal government.
“The good news for providers is, they would be much worse without this,” Tumlinson said, adding that specifying dollars for HCBS could relieve pressure on states and guard against additional rate cuts for assisted living providers.
Modernizing eligibility
A second recommendation in the blueprint is to modernize long-standing Medicaid eligibility policies. Current policy “creates a bias toward institutional care, making it difficult for individuals to remain in their home or the community,” including assisted living communities that are home to many older adults, when there is a need for LTSS.
Immediate ways to meet this recommendation include changing eligibility to increase access to HCBS in the most appropriate care setting, according to the report. Longer-term ways to meet the recommendation include applying minimum 1915(c) eligibility standards across states to reduce inequity and improve access.
Workforce investment
Investing in the direct care workforce delivering HCBS is the third recommendation in the blueprint. Direct care workers historically work demanding jobs with low wages, the report noted. ATI recommends that policymakers take a “comprehensive approach to fairly compensate, elevate and retain, engage and develop workers.”
In the short term, suggestions from ATI on ways to accomplish this recommendation include increasing wages, creating a federal direct care office, investing in training, and launching a public service campaign to address key workforce issues.
Longer-term measures include enhancing policies to support affordable childcare, healthcare and paid sick leave. The report also suggests modernizing training and creating a permanent federal Center for Direct Care Excellence.




