DALLAS — With increasing acuity levels among residents, many assisted living communities are seeking partners to help them integrate care through home health, therapy and other offerings. Maria Nadelstumph, vice president of organizational development and program excellence at Mt. Laurel, NJ-based Brandywine Living, shared five lessons her company has learned through its experience during a Thursday session at the National Investment Center for Seniors Housing & Care’s Spring Investment Forum.
Find the right partner.
“We have been working with a variety of partners, but finding the right partner is truly key,” Nadelstumph said, adding that the best partners complement a senior living organization’s brand and share the same values.
“Our resident is their patient, so we’re working together on this shared mission to make sure people are healthy and out of the hospital and staying at home,” she said.
Senior living executives must gain access to C-suite executives at the organizations with which they want to partner, Nadelstumph said. “You have to go in at the top in order to get that buy-in and then work from there,” she added.
Educate that assisted living is “home.”
Educating potential partners that assisted living is “home” to many older adults “is probably one of the biggest things that we’ve been challenged with,” Nadelstumph said. “The hospital systems as well as the providers are still unsure of what assisted living is, still unsure of what we can provide.”
Beyond just talking in a boardroom, however, she said, “We have to get people into the communities to see what we’re about.”
Define the scope of services.
Operators must determine not just what services will be offered but also how they will be implemented, Nadelstumph said.
“It’s not one-size-fits-all. It’s very customized,” she said. “It’s what works for the individual community, what the consumer needs are and what we can do and what we can handle.”
One community may offer a whole suite of services — a geriatrician on site or a consulting medical director, on-site therapy and fitness classes — whereas another might have more limited offerings such as a home health provider, Nadelstumph said.
“What we learned is that we had to spend more time on phasing things in and really coming up with a true integration plan to create that stickiness,” she said. “If you’re going to bring services in, make sure you have detail behind it, a roadmap on how to roll it out.”
Market the partnership.
“We can design beautiful brochures — and we’re proud of what we design — but the reality is, people really want to know the real stories,” Nadelstumph said. “We spend more time now talking to the individuals who are getting the care and also after care.”
One testimonial, she said, might relay the story of an 85-year-old who moved into a community relying on a cane or a walker but now coordinates a walking club.
“We want to be able to showcase that quality of life, because that’s what we’re focused on,” Nadelstumph said. “Everyone’s definition of quality of life is different, but if you ask an 85-year-old, ‘How would you define quality of life?’ I’ll bet you they will say, ‘Help me maintain a level of functioning so I can stay connected to my family and friends. I want to stay connected to my hobbies, my interests and maybe try something new.’ ”
Track quality outcomes.
“We are at the NIC conference. Everybody is focused on data, data, data. Of course, we are, too,” Nadelstumph said. “But what we’re still trying to navigate through is, what outcomes matter the most? What should we be tracking, working with our healthcare partners who are getting that data at the same time? Not just what the data is, but how are we operationalizing what we learn? So we may look at rehospitalization rates, but at the same time, we take it back to the front line at the community level. We’ve got to get away from the spreadsheets; we’ve got to get the information down to the community level to make sure that were pushing what we learn out there for preventive healthcare, so we’re not reactive but more proactive.”
Nadelstumph’s comments came as part of a panel discussion moderated by Rich Tinsley of Stoneridge Partners and including Anthony D’Alonzo, home healthcare director of Bayada Home Health Care; Hilary Forman, vice president and and chief clinical strategy officer at HealthPRO Heritage; and Daniel Fagan, vice president of population management for National Church Residences.
NIC day 2
In addition to other educational sessions, Thursday’s NIC conference featured an opening session about trends in healthcare payment and delivery reform and a lunchtime session about investment strategies in senior living and skilled nursing.
NIC President and CEO Brian Jurutka said that the meeting has drawn almost 1,800 attendees, a mix of operators and developers, capital providers, transactional and nontransactional professionals and a newer category of “senior care enablers” such as insurance, podiatry, and physician group representatives.
The NIC Spring Investment Forum ends Friday.
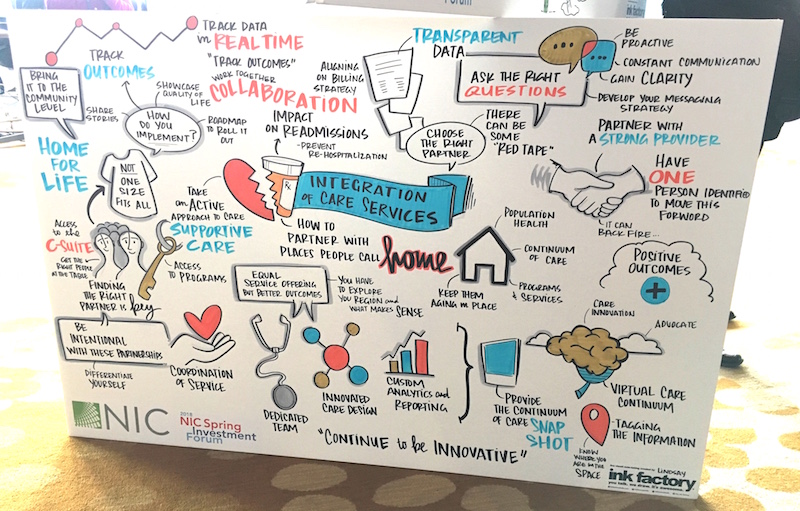
Below, an artist’s depiction of the session. The poster was made as panelists spoke.