A majority (64%) of senior living communities reported no COVID-19 deaths in 2020, according to an analysis of COVID-19 deaths across the long-term care residential continuum released today.
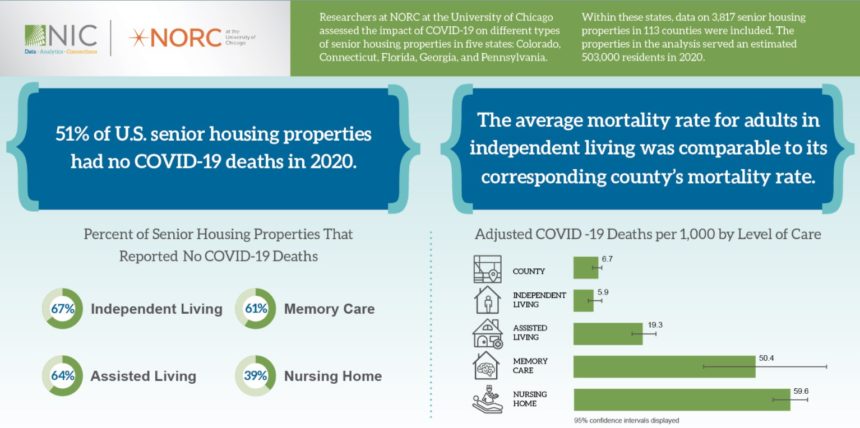
The National Investment Center for Seniors Housing & Care provided grant funding to NORC at the University of Chicago to examine mortality rates by property type. The analysis found that 67% of independent living communities, 64% of assisted living properties and 61% of memory care communities studied saw no COVID-19-related deaths in the 10 months of 2020 that COVID was known to be present in long-term care. Overall, including all senior living communities (independent living, assisted living and memory care), 64% saw no COVID-19 cases, according to researchers.
“While COVID-19 has been devastating for older adults, a majority of properties avoided any resident deaths,” Caroline Pearson, NORC senior vice president of healthcare strategy and lead researcher, said in a statement.
The average mortality rate for residents in independent living was statistically the same as the mortality rate of the overall 75-and-older general population, according to the analysis, suggesting that independent living residents were not at higher risk of death from COVID-19 than were their peers living in private homes in the greater community.
The mortality rate at assisted living properties was one-third that of skilled nursing facilities, where only 39% of properties had no deaths due to COVID. With SNFs included in the overall calculation, 51% of all types of long-term care facilities did not have a case of COVID-19.
“Death rates in senior housing increased in settings of care that serve the most vulnerable residents, based on age, health status and caregiving needs,” Pearson said.
The highest mortality rate by percentage occurred in SNFs, followed by memory care; in both settings, severity of illness and complexity of caregiving needs are higher. The analysis also found that memory care units faced particular challenges with infection control because residents, who have cognitive impairments, are more likely to require additional care and support for their basic needs.
“Ultimately, every COVID-19 death in any community designed for older adults is tragic, and lessons were learned regarding health and safety protocols and where improvements are most needed,” NIC President and CEO Brian Jurutka said in a statement. “The facts include that COVID-19 transmission is more likely with close person-to-person contact and mortality increase with age and comorbidities. This study shows senior housing isn’t homogenous, and mortality was higher in property types whose residents, on average, are sicker and require higher levels of care.”
Advisers to the NORC study — among them Bob Kramer, NIC co-founder and strategic adviser as well as founder and fellow of Nexus Insights, and Kevin O’Neil, M.D., ALG Senior’s chief medical officer — said that further research is needed to better understand the role that health, age and demographics play in mortality rates by different congregate care settings. NIC indicated that it will support a second phase of research — to be completed in November — to build on this study’s findings and to improve the general public’s understanding of the safety levels within the various senior housing and care segments.
The research, co-sponsored by the John A. Hartford Foundation, included data from 3,817 senior living and care properties across 113 counties in five states: Colorado, Connecticut, Florida, Georgia and Pennsylvania. The study also included a dozen interviews with senior housing and care operators and eight state affiliates or state partners of LeadingAge or Argentum.




