
The percentage of nursing home residents who are considered “low care” increased 54% between 2019 and 2020, representing an opportunity for assisted living providers, according to a new report.
Low-care nursing home residents are those who require no physical assistance in bed mobility and activities of daily living such as transferring, toileting and eating. Such residents may be able to live in less restrictive environments and receive less-intensive care in assisted living communities and other alternative settings or through home- or community-based services, according to the authors of America’s Health Rankings’ “Senior Report 2022,” published by the United Health Foundation. The data they cited about low-care nursing home residents came from the Brown University Shaping Long-Term Care in American Project.
Nationally, the authors said, the percentage of nursing home residents who are considered low care increased from 9.9% to 15.2% from 2019 to 2020, reaching its highest point in the 10-year history of the report. Before the recent increase, according to the report, the percentage of low-care nursing home residents decreased 19%, going from a total of 12.2% to 9.9% of all nursing home residents, between 2010 and 2019.
The percentage of low-care nursing home residents increased in 49 states (no data were available for Alaska), and in 44 states the increase was by 25% or more. Leading the way were Utah (a 181% increase, going from 3.6% to 10.1% of all nursing home residents), Ohio (134%, from 6.8% to 15.9%) and North Carolina (133%, from 4.6% to 10.7%).
The percentage of low-care nursing home residents among all nursing home residents was the highest in Missouri (31.3%), Oklahoma (28.3%) and Kansas (26.0%), and it was the lowest in Hawaii (3.7%), Maine (4.4%) and South Carolina (7.9%).
The report provides a portrait of the health and well-being of older adults in the United States and features long-term trends and disparities across demographic subpopulations meant to spark dialogue and action to improve senior health across the nation and on a state-by-state basis.
“In 2020, there were more than 55.6 million adults ages 65 and older in the United States, making up approximately 16.9% of the population. This number is expected to rise to 73.1 million, or 21% of the population, by 2030 when the last of the baby boomer generation ages into older adulthood,” the authors wrote. “At that point, more than 1 in 5 people in the U.S. will be of retirement age. Thus, it is essential that policymakers, community leaders and public health officials consider how to best safeguard and improve the health of older Americans.”
States ranked
Maine, Florida and West Virginia had the highest percentage of older adults in 2020, according to the report.
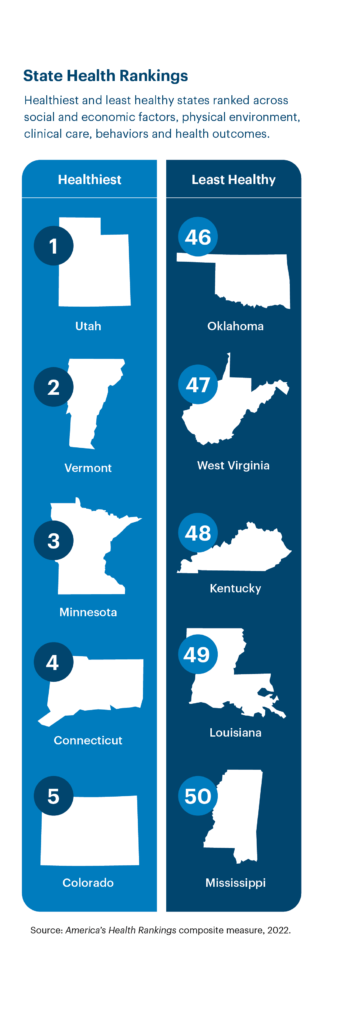
In overall state rankings in the report, based on 37 measures across five categories of health, Utah was ranked the healthiest state, and Mississippi was rated the least healthiest state.
Utah ranked in the top quintile across social and economic factors (No. 1), clinical care (No. 8), behaviors (No. 4) and health outcomes (No. 4) categories. Strengths in the state included a low prevalence of excessive drinking, a low risk of social isolation and a low prevalence of smoking. Challenges in Utah included a high prevalence of falls, low Supplemental Nutrition Assistance Program participation among older adults living in poverty and a low geriatric provider rate.
Mississippi ranked in the bottom quintile across all model categories: social and economic factors (No. 50), physical environment (No. 44), clinical care (No. 49), behaviors (No. 47) and health outcomes (No. 43). Strengths in the state included a low prevalence of excessive drinking, a low prevalence of falls and a low prevalence of severe housing problems. Challenges in Mississippi included a high early death rate, a high risk of social isolation and a high prevalence of physical inactivity.
For additional coverage of the Senior Report, see McKnight’s Home Care.



