Governors and public health officials should ensure that residents and employees of long-term care facilities are prioritized before everyone else for COVID-19 vaccination and that they receive both doses of the vaccine by March 1, American Health Care Association/National Center for Assisted Living executives said Monday.
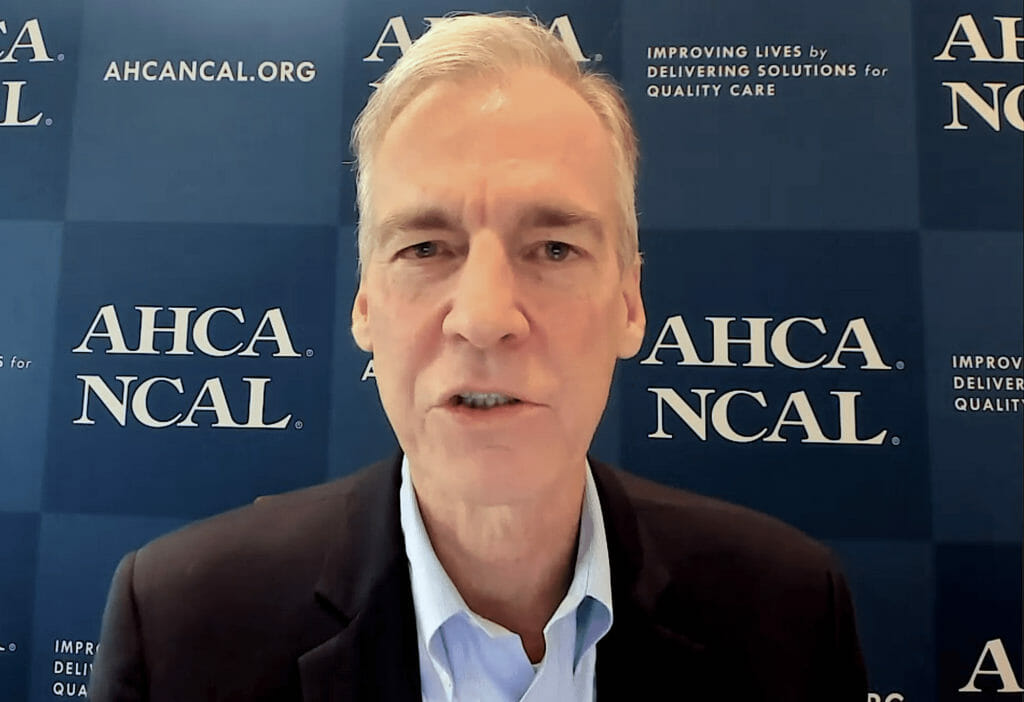
“It is a staggering statistic that less than one percent of the COVID cases in the United States have hit people in long-term care but over 40 percent of the deaths have occurred there,” AHCA/NCAL President and CEO Mark Parkinson said on a call with members of the media. “And as tragic as that statistic is, it gives us an incredible opportunity to make a huge difference in the mortality rate, just by focusing the initial rounds of vaccine distribution and actual vaccination on this very vulnerable population.”
Approximately 5,000 deaths per week are occurring due to COVID across independent living and assisted living communities and skilled nursing facilities, and more than 1,000 long-term care workers have died from the virus, Parkinson noted. Fortunately, he said, so far, state and local officials making decisions about whom to prioritize for the limited amount of vaccine that will be available at first appear to agree with a recommendation, made last week by the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices, that long-term care residents and staff, as well as healthcare personnel, be the top priorities.
Any government official not deciding to vaccinate long-term care residents and employees first, Parkinson said, would be making “an enormous public health blunder,” even if it means that healthcare workers outside of long-term care have to wait to be vaccinated.
“We’re not in any way suggesting that there are healthcare workers that are in that top tier that shouldn’t be vaccinated. We totally get that,” he said. “But what we are saying is that with the limited supply that’s going to be available over the next few weeks, the absolute top of that top tier should be long-term care facility residents and the folks that take care of them. And the reason is because of the realities of the data that just clearly demonstrate that if we can do this, if we can get this done in the next 60 days, we can cut the overall COVID death rate by 40% just by getting those initial four or five million doses out to that very important population.”
Vaccine could be ready Dec. 21 or 28
Exactly when the vaccine will be available to long-term care residents and staff, AHCA/NCAL Chief Medical Officer David Gifford, M.D., MPH, said, depends on whether and how quickly the Food and Drug Administration grants emergency use authorization for the Pfizer and Moderna formulations. AHCA/NCAL and others are proceeding with the assumption that the vaccine will be ready for long-term care recipients by Dec. 21 or 28, he added. That timing, however, could be pushed back if FDA emergency use authorization is not granted or is delayed, Gifford said.
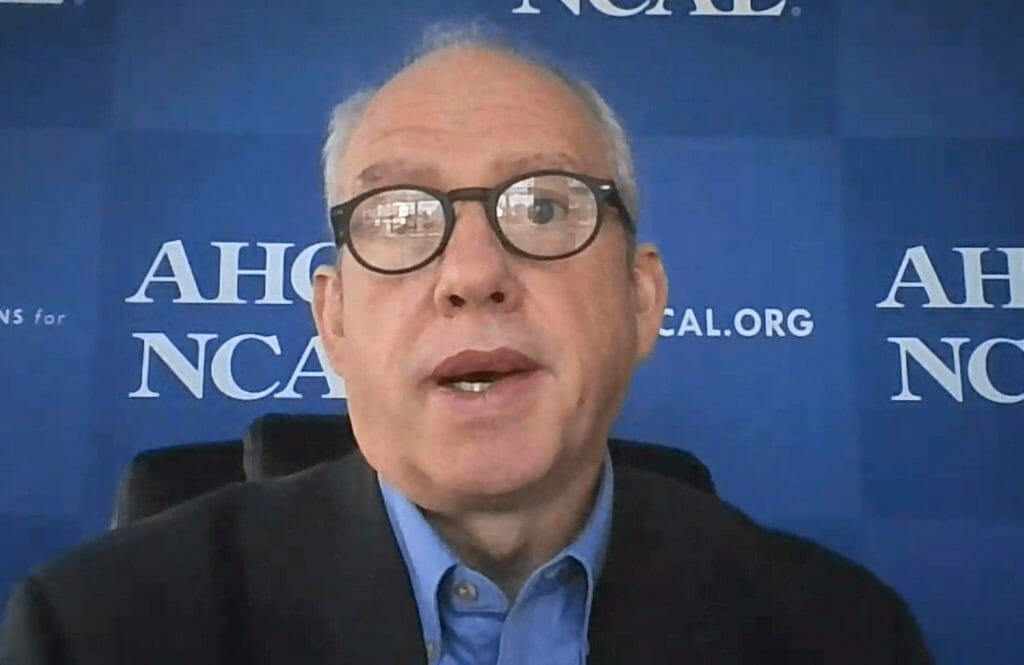
Both vaccines require two doses, spaced a few weeks apart, meaning that AHCA/NCAL’s request could leave approximately two months for residents and staff members to be vaccinated. But whenever the vaccine is ready, Gifford said that AHCA/NCAL anticipates that residents and employees will be eager to take it.
“A lot of families and residents are really worried about this virus, and so they’re really excited and looking forward to … getting the vaccine, because of that concern. The same with the staff; the staff are having to get tested, often twice a week, and having to stay out of work because of the virus,” he said. “They’re seeing family members in the community get sick. They’re seeing the residents get sick. So … they are very sort of excited about the vaccine.”
Parkinson said that although some residents and workers may hesitate to be vaccinated, “I don’t think it will be anywhere near the kind of numbers that you see in the public polling about resistance to the vaccine. Tragically, our people have seen upfront how horrible this virus can be, and so I would assume that the adoption rates would be much higher among workers and residents in facilities.”
Mandates not expected
Gifford said he doesn’t foresee federal or state mandates for vaccination. As to whether AHCA/NCAL would support a long-term care employer mandate of the vaccine, Parkinson said: “We are waiting to see what kind of acceptance rate we get among employees. There are some legal questions about whether or not there can be a mandated use of a vaccine that’s under emergency use authorization as opposed to under normal authorization.
“Our hope is that we get widespread acceptance of the vaccine, but if we don’t, I assure you that our organization, as well as individual operators, will be analyzing whether or not they can mandate the vaccine,” he continued. “We’re just hoping that we don’t have to go there.”
Even though the vaccine trials have not included many people in their 80s, a typical age for long-term care residents, Gifford said, “As a physician and as a child of parents who are in their 80s, I am not worried at all about recommending this vaccine to someone in our group out there.”



