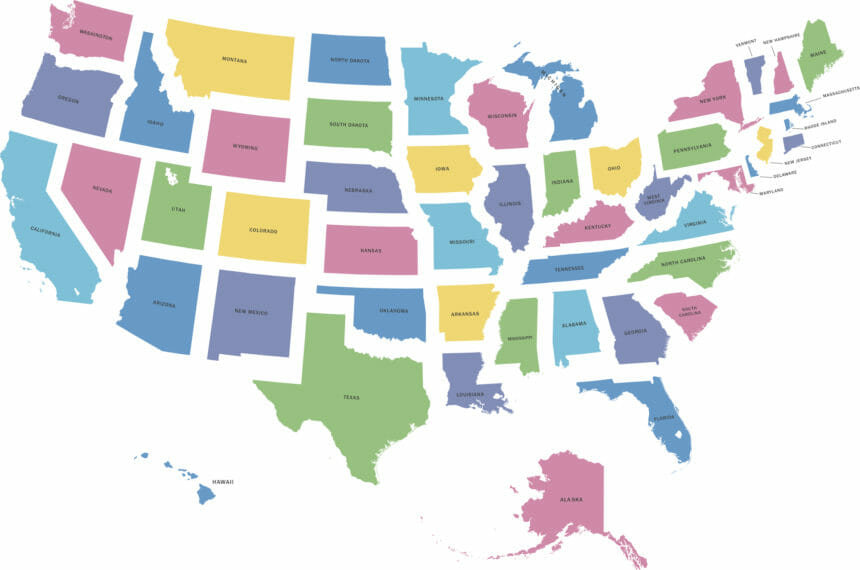
Multistate senior living operators have much to stay on top of as some states impose new COVID-related measures amid federal masking recommendations and increased transmission rates from virus variants, whereas other states move to prohibit such measures. And even operators with business limited to one state can be hampered by state orders, laws and regulations that dictate how they respond to the pandemic.
The moves by states are happening as the White House on Friday announced that federal employees and onsite contractors must get the shot or wear a mask and submit to weekly testing. President Biden also called on states and local governments to offer $100 vaccine incentives to unvaccinated individuals. Colorado, New Mexico and Ohio all are offering such an enticement.
COVID-19 vaccine mandates
Monday, New Jersey Gov. Phil Murphy (D) announced a COVID-19 vaccine requirement for certain state and private healthcare facilities and high-risk congregate settings, including assisted living communities. Employees in those settings will be required to be fully vaccinated against the coronavirus or be subject to a minimum level of weekly COVID-19 testing.
“While reaching our statewide vaccination goal has so far dampened the impact of the Delta variant in New Jersey, some of our most vulnerable populations remain at risk for serious illness or death from COVID-19, primarily due to exposure to unvaccinated individuals,” Murphy said. “Individuals in healthcare facilities should have confidence in their caretakers, and this measure will help ensure peace of mind for those in higher-risk settings.”
Murphy added that he is prepared to consider additional measures “if we do not see a satisfactory increase in vaccination uptake in those settings.” Affected workers have until Sept. 7 to comply.
Meagan Glaser, vice president of LeadingAge New Jersey & Delaware, told McKnight’s Senior Living that it joins the national LeadingAge affiliate in supporting vaccine mandates for long-term care workers. Members have worked to help members “educate, promote and offer the COVID-19 vaccine to their staff and residents,” she added.
“Consequently, an overwhelming majority of our residents have been vaccinated, and staff vaccination rates continue to increase,” Glaser said. “However, as new variants of COVID arise and proliferate, LANJDE strongly urges all residents and staff in long-term care to get vaccinated.”
Health Care Association of New Jersey President and CEO Andy Aronson said the organization “strongly urges” vaccination of all healthcare personnel.
“Our residents and their families deserve the comfort of knowing that their caregivers are vaccinated,” Aronson told McKnight’s Senior Living. “We welcome this pledge by the governor to work with union and labor leaders to help us move closer to this goal. Together we can help to provide the full level of protection that our residents deserve.”
HCANJ is the state affiliate of Argentum and the American Health Care Association / National Center for Assisted Living. AHCA / NCAL “strongly urges” vaccination against COVID-19 for all healthcare personnel and supports all providers that adopt mandatory COVID-19 vaccination policies for such workers.
On the other side of the country, California became the first state last week to require all state workers, as well as workers in long-term care and other healthcare settings, to get a COVID-19 vaccine or undergo weekly testing.
And in Colorado, the Department of Public Health and Environment extended existing public health orders and amended another requiring face masks in locations serving vulnerable populations. The amendment, which is in effect Aug. 1 through Sept. 1, recommends that all unvaccinated staff members test daily with a rapid test and/or weekly with a PCR test. The public health order requiring masks in assisted living communities, skilled nursing facilities, intermediate care facilities and group homes remains in place.
Last week, Virginia Gov. Ralph Northam (D) tweeted that all Virginians should wear masks in public indoor settings where increased risk of COVID-19 transmission exists.
And at a news conference Thursday, North Carolina Gov. Roy Cooper (D) applauded businesses implementing vaccine mandates. The state, he said, is “at a crossroads in the pandemic,” and he encouraged private businesses to mandate vaccination.
Cooper also encouraged anyone living in a county with a high spread rate of the coronavirus to wear a mask in public settings indoors. He also directed state government cabinet agencies to verify employee vaccination status. Unvaccinated employees will be subject to weekly COVID-19 testing. He encouraged other state agencies and private businesses to adopt similar policies.
New York City Mayor Bill de Blasio (D) announced last week that all city workers must be vaccinated by Sept. 13 or submit to weekly COVID-19 testing. The announcement followed a similar mandate issued the week prior for the city’s public healthcare workers in congregate and residential settings, including senior living communities, as well as city-run hospitals and clinics.
Affecting multiple states, the federal Department of Veterans Affairs became the first federal agency to implement a coronavirus vaccine mandate.
Not so fast
Operators in some states need to read the fine print to see whether government actions limit their pandemic responses.
Texas Gov. Greg Abbott (R) issued an executive order last week combining several existing COVID-19 executive orders that emphasize a “path forward that relies on personal responsibility rather than government mandates.” The new order effectively prevents local and state governments from imposing mask or vaccination mandates; those that do will face a $1,000 fine. The state also is prohibiting public and private entities that receive public funds from requesting someone’s vaccination status as a condition for entry.
Assisted living communities, hospitals and jails, however, are exempted from the order and “may continue to use appropriate policies regarding the wearing of face coverings,” the governor said. Assisted living communities and nursing homes also will still be able to require documentation of a resident’s vaccination status.
Carmen Tilton, Texas Assisted Living Association vice president of public policy, told McKnight’s Senior Living that Abbott’s executive order doesn’t change current policy for assisted living operators.
What the order does do, Tilton said, is it “effectively restricts local jurisdictions from creating local standards which are more restrictive than the executive order’s language, with regards to face masks and vaccines.”
“In this regard, the executive order establishes a consistent state guidance which covers all jurisdictions, while continuing to allow assisted living communities to develop their own infection control and vaccination policies,” Tilton said.
Meanwhile, in Montana, the state Department of Labor and Industry issued guidance last week to help employers comply with a new law that says they can’t mandate COVID-19 vaccinations. Assisted living communities and other long-term care settings are exempt. House Bill 702, which was signed into law on May 7, was amended by Gov. Greg Gianforte (R) to grant exemptions for assisted living and other long-term care facilities over concerns that complying with the law would put them out of compliance with federal regulations.
And in Oregon, a 32-year-old law might prevent some operators from moving forward on vaccine mandates for some workers. The law explicitly prohibits healthcare organizations from mandating vaccinations for workers. Senior living associations in the state said the law prohibits operators from requiring a vaccine of licensed staff members, including certified nurse assistants, nurses and administrators. But operators may be able to mandate vaccines for non-licensed staff members.




