The federal government is making $25.5 billion in new funding available to healthcare providers, including assisted living operators, affected by the COVID-19 pandemic.
The U.S. Department of Health and Human Services announced today that it is making the funding available through the Health Resources and Services Administration. The funding includes $17 billion in Phase 4 Provider Relief Funds covering a broad range of providers — including assisted living companies — that can document revenue losses and expenses associated with the pandemic.
Another $8.5 billion in American Rescue Plan funding will go to providers who serve Medicaid, Children’s Health Insurance Program or Medicare beneficiaries in rural locations.
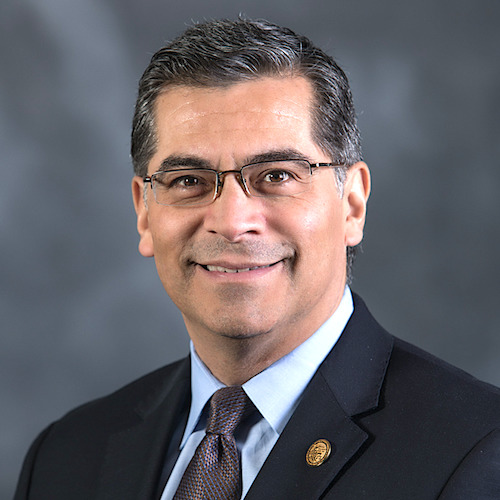
“This funding critically helps healthcare providers who have endured demanding workloads and significant financial strains amidst the pandemic,” HHS Secretary Xavier Becerra said in a statement. “The funding will be distributed with an eye towards equity, to ensure providers who serve our most vulnerable communities will receive the support they need.”
Phase 4 Provider Relief Fund payments will be based on providers’ lost revenues and expenditures between July 1, 2020, and March 31, 2021. The funds will reimburse smaller providers for lost revenues and COVID-19 expenses at a higher rate compared with larger providers, according to HHS.
Phase 4 distributions also will include bonus payments for providers who serve Medicaid, CHIP and / or Medicare beneficiaries who are of lower income and have more complex medical needs. HRSA will price the bonus payments at the higher Medicare rates to ensure equity for those serving low-income older adults, people with disabilities, pregnant women and children.
The application portal will open Sept. 29.
HHS also released detailed information about the methodology used to calculate Phase 3 Provider Relief Fund payments. Providers who believe their Phase 3 payment was not calculated correctly now have an opportunity to request reconsideration. More details on that process will be shared at a later date, HHS said.
HHS also announced a final 60-day grace period to help providers come into compliance with Provider Relief Fund reporting requirements if they fail to meet the Sept. 30 deadline for the first reporting period. Although the deadlines to use funds and the reporting time period will not change, HHS said it will not initiate collection activities or similar enforcement actions for non compliant providers during the grace period.
More information can be found on the HRSA website.




