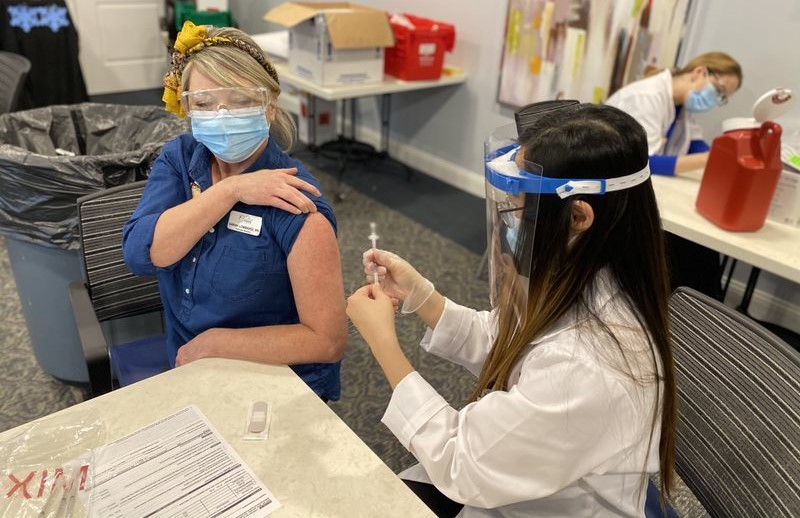
Explaining the science behind the development of the COVID-19 vaccinations as well as the community benefit of getting vaccinated helped EvergreenHealth, a home care provider in Washington State, attain an employee vaccination rate of around 87%.
From the beginning, leaders told employees that if vaccination information doesn’t come from a doctor, someone with a degree in public health or a person in the scientific community, “it shouldn’t be listened to,” said Brent Korte, chief home care officer for EvergreenHealth, of Kirkland, WA, who spoke Wednesday during a town hall on pandemic lessons. The National Association for Home Care & Hospice sponsored the town hall.
Also helpful to impart to employees is that the reason the vaccines emerged so quickly was because of the frequency of the virus. Because so many people contracted COVID-19, unlike other outbreaks, such as the Ebola virus, the government could “do their trials more quickly,” Korte said.
There is one way to combat misinformation and rumors, he said: “science, science, science.”
Vaccine hesitancy has been a major obstacle in the vaccination effort among healthcare employees. A recent Washington Post/Kaiser Family Foundation poll found that more than 1 in 3 frontline healthcare workers said they were not confident the vaccines had been adequately tested. Only 26% of home care workers have been vaccinated, according to the poll.
Telling the employees that getting vaccinated has a larger community purpose has been another effective line of argument, Korte said. Using the metaphor that the vaccine is creating a wall against the virus and every brick, or vaccinated person, is necessary, has hit home. The organization also has explained that getting vaccinated is good for job security, because the organization benefits, he said.
Leadership attributes
Reflecting on the last year, presenters said the pandemic helped to sharpen certain skill sets. Practicing daily incident command coordination and response was a skill the crisis helped hone, said Denise Schrader, RN, vice president of integrative services for Mosaic Life Care Hospice & Palliative Care, of St. Joseph, Missouri.
“We can do it in our sleep now,” she said.
Having to keep up with constant change and then translate that into procedures for the safety of patients, staff, families and others was “almost like a rapid fire,” she said.
The enormous effort required during the last year to maintain operations has taken a toll on staff and leadership, both Schrader and Korte said.
Going forward, healthcare leaders have to start planning now to address issues of staff fatigue, general exhaustion and burnout from the front line to leadership, according to Korte.
“Our work as healthcare leaders really is just getting started,” he said.




