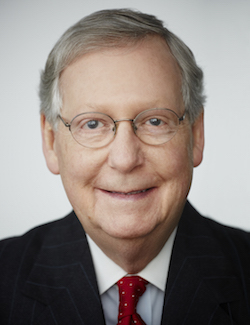
The 74 million lower-income, disabled and older adults who rely on Medicaid for their healthcare coverage could be harmed, and the healthcare system unduly burdened, under current proposals to replace the Affordable Care Act, the leaders of 10 large managed care organizations said Tuesday in a letter to Senate Majority Leader Mitch McConnell (R-KY) and Minority Leader Chuck Schumer (D-NY).
The health plans represent almost 13.5 million Medicaid beneficiaries in 23 states.
The company presidents and CEOs said their main concerns with discussions around the American Health Care Act lie with Medicaid. The formula proposed to determine funding limits under a system of capped Medicaid payments to states, they wrote, “would amount to a 25 percent shortfall in covering the actual cost of providing care to our nation’s neediest citizens” by 2026.
“Although current federal matching funds for Medicaid are open-ended, states must balance their own budgets, giving them strong incentives to control costs and ensure program integrity,” they said, noting that many services already are provided through managed care organizations “to minimize costs while maximizing outcomes.”
“There are no hidden efficiencies that states can use to address gaps of this magnitude without harming beneficiaries or imposing undue burden to our healthcare system and all U.S. taxpayers,” they said.
The letter authors said they seek “meaningful Medicaid reform,” not maintenance of the status quo, but that they oppose the Medicaid proposals being debated in the Senate.
“A well-considered Medicaid reform proposal is necessary for this vital program to continue to provide access to quality healthcare for vulnerable populations and the safety-net providers who serve them,” they said.
The CEOs said they welcome the opportunity to work with the government to increase efficiency in the Medicaid program. Among their ideas are regulatory simplification, increased waiver flexibility for states, value-based pricing, and consolidation of administration and benefit design for dually eligible individuals.
Companies represented by the letter include AmeriHealth Caritas, Blue Shield of California, CalOptima, CareSource, Gateway Health Plan, Healthfirst (NY), Inland Empire Health Plan, LA Care Health Plan, Molina Healthcare and UPMC for You.



