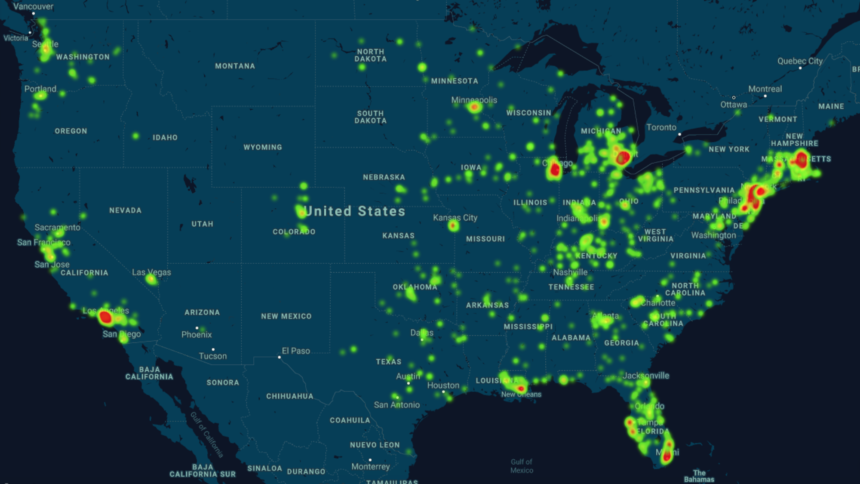
Two associations behind a new “heat map” that visually conveys the prevalence of COVID-19 within assisted living communities and nursing homes across the country say it should help providers make the case for more personal protective equipment, testing and even staffing and additional capacity, if needed, to prevent or contain the spread of the disease.

“We need to know what the picture is for post-acute long-term care, and I think with this heat map, there’s an immediacy about seeing that visual picture,” Christopher E. Laxton, CAE, executive director of AMDA – The Society for Post-Acute and Long-Term Care Medicine, told McKnight’s Senior Living. “We’re hoping it’ll really help providers advocate for themselves when they’re in discussions with their local healthcare partners and the local health authorities.”
AMDA and pharmacist association ASCP collaborated on the tool. It uses publicly available information released by states, as well as information sourced by members of both organizations. (AMDA members are encouraged to contribute data at https://profile.paltc.org/COVID19-USA-Heat-Map — member login is required.)
A general heat map displays the presence of COVID-19 at a ZIP code level, and users also can look at the map by region. Only COVID-19-related fatalities are included for Alaska, Arizona, Hawaii, Idaho, Mississippi, New Hampshire, New Mexico, New York, North Carolina, Texas, Utah and Wisconsin.
Although more skilled nursing data are available right now compared with assisted living data, and not all states are represented, Laxton said that AMDA and ASCP hope both types of operators also will find the data via the map helpful for advocacy at the national level.
Some senior living associations recently expressed frustration at federal and state government plans to exclude independent living, assisted living, memory care and continuing care retirement communities from an upcoming distribution of PPE.
“I’m very worried about assisted living, senior living. It is sort of the forgotten side of post-acute long-term care when it comes to COVID, and truthfully, it’s probably an inheritance from many, many years of assisted living not wanting to see itself as a healthcare setting,” Laxton said. “But the resident population in assisted living communities really tracks very closely with the resident population in nursing homes. The frailty, the multiple comorbidities — all of the issues that challenge nursing home populations with respect to the transmissibility of this virus — those apply just as much to the assisted living world as they do to the nursing home world.”
Most people remain unaware of the similarity — and the difference, he said.
“And I’m not talking about the general public here. I’m talking about healthcare, where to them, everything is a nursing home, and that’s just not the case,” Laxton said. “So I really hope that assisted living begins to be included more in considerations for how to prioritize PPE for staff, how to prioritize testing for residents and, again, the need for medical oversight. This is a position AMDA has had for some time now and one that this just shines a very bright light on.”
Within the next two weeks, the Centers for Disease Control and Prevention also is expected to make public its data from assisted living communities and nursing homes. At that time, the heat map will be updated from this data source, according to the associations.
“There will be a rollout time, getting people used to understanding what’s required and what they need to do to participate,” Laxton said. “In the end, perhaps in a month from now, that heat map will be much more complete, and it will show suspected and confirmed cases as well as COVID deaths.”
Editor’s note: The CDC’s National Healthcare Safety Network LTCF COVID-19 Module is now online. Facilities eligible to report include assisted living communities, nursing homes / skilled nursing facilities, and facilities providing long-term care for the developmentally disabled.



