COVID-19 is the biggest crisis to hit the long-term care industry in its history, but the question now is how to ensure that providers are prepared should something like it happen again, Mark Parkinson, president and CEO of the American Health Care Association / National Center for Assisted Living said while opening LeadingAge’s 15th Annual Collaborative Care HIT Summit. The meeting went virtual this year due to the pandemic.
Part of the answer, he said, lies in technology.
The effect of COVID-19 on the long-term care industry is “historic and tragic,” in large part due to the “unthinkable amount of death — both residents and staff members,” he said.

“How did this happen, and what can we do to keep it from happening in the future?” Parkinson asked. “It’s very important to understand moving forward what did happen here so we can understand the right policy and process solutions to keep this from happening in the future.”
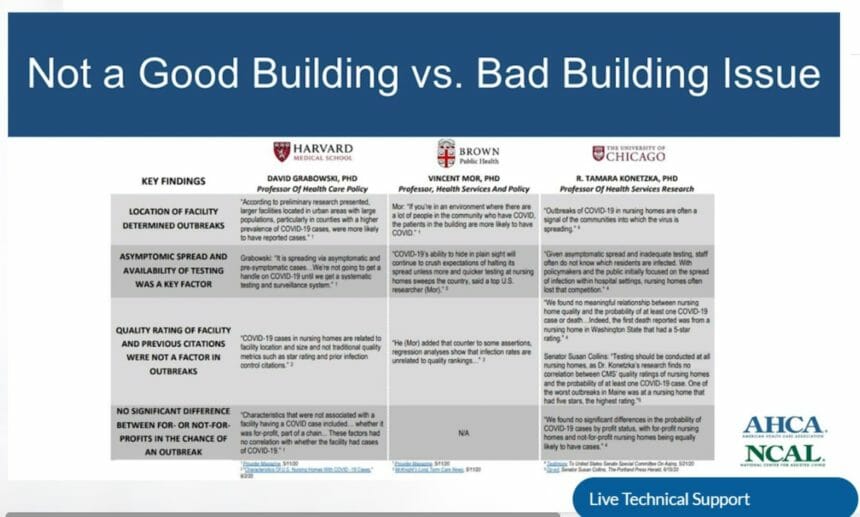
The pandemic, he said, will produce a deep analysis of long-term care, as it should. Critics, however, will simplify the situation to one of “good” buildings versus “bad” buildings, Parkinson added.
Independent studies from Harvard University, Brown University and the University of Chicago have found no correlation between a five-star nursing home rating, prior infection control performance or staffing levels and the incidence of COVID-19 in buildings, he pointed out.
“The only strong correlation between whether a building got COVID or not was whether or not it was in a community that had a bunch of COVID,” Parkinson said.
“Perfect infection control” didn’t stop the virus from entering a building, because in the early months of the pandemic, no one knew that asymptomatic carriers would be a major source of that transmission, he said.
“It’s not a reflection of the fact that we’re terrible at what we do. We don’t need more fines, we don’t need more penalties, we don’t need more criticism,” Parkinson said. “What we need instead is a real analysis of what can and should be done to prevent this in the future.”
For more than a decade, Parkinson, said the industry has complained that it should not have been left out of the American Recovery and Reinvestment Act of 2009, a government stimulus act that provided funding for information technology. He called it an “enormous policy mistake” that prevented IT from growing in long-term care.
But, he said, the “time for complaining is over.”
“That was more than 10 years ago, and yes, it was a horrendous policy mistake, but it happened, and it’s time for us to move on,” Parkinson said, adding that the industry should work with pioneers to create “real systems that bring us into the 21st century. “For us to most effectively take care of the folks in our buildings and most effectively collaborate with the rest of the healthcare system, we’ve got to continue and accelerate investments in IT.”
Long-term care, he said, has been isolated from the rest of the healthcare world for too long. The industry felt the “cruel impact” of that fact when priorities for testing and PPE during the pandemic were made. Collaboration and IT, he said, are two of the most important factors in helping the industry provide exceptional care to residents.
In other coronavirus-related news:
- House Speaker Nancy Pelosi (D-CA) announced Tuesday that the House of Representatives will remain in session until there is an agreement on another round of emergency coronavirus relief funding. In a conference call with the House Democratic Caucus, Pelosi, who is facing pressures from moderate Democrats to get a deal signed, said she isn’t willing to accept a “skinny” legislative package and said the chamber’s calendar will be extended until an agreement is sealed.
- Assisted living facilities in Florida no longer have to test staff for COVID-19 after two emergency mandates from the state Agency for Health Care Administration expired Sunday. Nursing home staff still are required to be tested under federal guidelines from the Centers for Medicare & Medicaid Services.
- Ohio Gov. Mike DeWine signed into law HB 606, known as the Good Samaritan Bill, which provides civil immunity to healthcare professionals in residential care facilities and other settings who unknowingly spread coronavirus in the workplace, unless the act constitutes reckless disregard for life or health. The protections will last retroactively from March 9, 2020, through Sept. 30, 2021.
- Advocates are calling for the Minnesota Department of Health to be transparent and release comprehensive COVID-19 data for long-term care facilities, including assisted living communities and nursing homes. The state lists exposures at care homes with 10 or more residents but does not include death data or numbers of infected individuals, citing federal health privacy laws for the lack of information.
- LeadingAge Pennsylvania is asking for another round of funding from the state’s remaining $1 billion in CARES Act funding to continue testing, paying hazard pay and providing personal protective equipment in the state’s long-term care facilities.




