
Editor’s Note, 10/29/21: The Urban Institute retracted this report after finding errors in order to re-examine the impacts.
Although the country depends on Medicaid as a safety net for people who need long-term services and supports, the current status of home- and community-based services does a “disservice to people who need care, their families and direct care workers,” according to a new report from the Urban Institute, which compares three potential funding options.
“Resources to support federal administration should, therefore, accompany a new commitment of federal dollars to state programs,” the authors wrote. “A significant boost in accountability and investment could advance the well-being of beneficiaries and their caregivers no matter where they live.”
The report comes as media reports indicate that President Biden’s plan to invest $400 billion in HCBS over eight years through an infrastructure bill may be in jeopardy.
Enhanced funding, the Urban Institute researchers determined, could substantially increase the adequacy of and equity in HCBS availability across the country, as well as improve the well-being of beneficiaries and their caregivers. Improvement, however, would require a commitment to the process, they said.
The effect of any enhanced HCBS funding for assisted living providers would depend on the location of the community and population served, according to Judy Feder, an Urban Institute fellow, public policy professor at the McCourt School of Public Policy at Georgetown University and one of the paper’s authors.
“There is no question it depends … on the eligibility terms and population a facility is serving,” she told McKnight’s Senior Living.
According to the report, about 14 million adults need significant help with LTSS, and the number of older adults with LTSS needs will increase by more than 60% by 2040.
Medicaid — the national’s “last resort financier of LTSS” — only funds services for low-income individuals, forcing many older adults to spend down their resources. Medicaid’s LTSS protections also vary by state. Only about 30% of older adults with significant LTSS needs rely fully or partially on care from paid workers, according to the report. One in six assisted living residents relies on Medicaid for their daily care, according to the National Center for Assisted Living.
Despite significant improvements in HCBS in most states over the past decade, the researchers stated, inadequacies and variation persist. Those variations reveal that the share of Medicaid LTSS funding spent on HCBS can range from an average of 33% in the first lowest HCBS spending states to 77% in the five states with the highest spending. Half of states spent 52.7% or more of their LTSS funds on HCBS.
Options
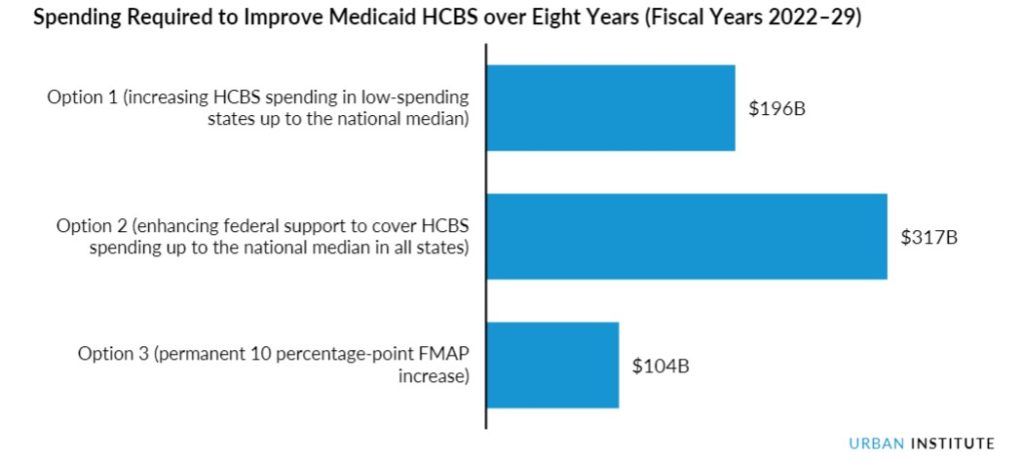
In one funding approach suggested by the researchers, permanently increasing each state’s federal medical assistance percentage by 10 percentage points would increase federal spending by about $104 billion over eight years. In the first year, authors stated, the approach could serve as many as 360,000 new beneficiaries while increasing annual wages by an average of $5,000 for 1.16 million workers.
A second approach would target federal dollars to bring low-spending states’ HCBS spending up to the national median. Doing so would increase federal Medicaid HCBS spending by a projected $196 billion over eight years and could reach 970,000 more beneficiaries in these states. This option also could increase wages by $5,800 per year for 400,000 workers in states with below-median HCBS spending.
A third option suggests providing new federal funding to all states — lifting low HCBS spending up to the national median and covering all state spending in higher-sending states up to that median. That option would increase federal costs by approximately $317 billion over eight years and could reach up to 1.1 million more beneficiaries across all states. It also could increase annual wages by an average of $5,000 for 1.46 million workers.




