COVID-19 cases deaths among assisted living and nursing home residents and staff members have fallen dramatically since vaccines were introduced in December, with deaths declining by almost 89% and cases by nearly 92%, according to a Kaiser Family Foundation analysis.
Eight states are reporting increases in long-term care cases, however, reflecting a potentially troubling trend of increasing community spread.
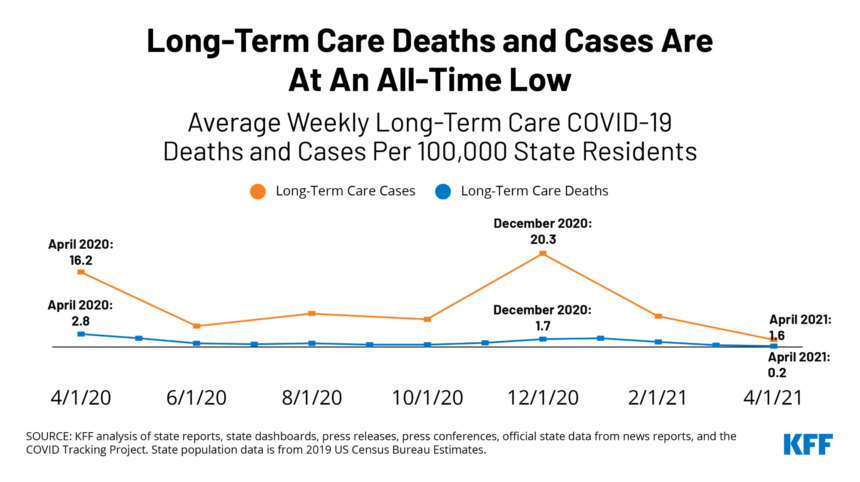
The KFF analysis found that COVID-19 deaths in assisted living communities, nursing homes and other congregate care settings fell from 1.7 deaths per 100,000 state residents in December to just 0.2 deaths per 100,000 residents in April — an all-time low, according to the KFF analysis.
Of the 38 states, plus the District of Columbia, for which trend data were available, 21 states reported all-time low death rates in April. Declines ranged from 68% in Virginia to 100% in Kentucky. Iowa was the only state that reported higher average weekly long-term care facility deaths in April than December — a 24% increase.
Thirty-six states in the analysis reported a greater than 80% drop in long-term care facility cases from December to April, with three states reporting at least a 50% drop.
More than 1.4 million residents and more than 1 million staff members in long-term care facilities are fully vaccinated.
Both nationally, and in most states the share of deaths attributed to long-term care facilities dropped since vaccinations between in December, indicating a faster decline in death rates in these facilities than in the community at large, according to the KFF analysis.
By mid-April, about one-third (34%) of all COVID-19 deaths were in long-term care facilities, down from a peak of nearly half (49%) in June. Only four states — Colorado (1%), Indiana (4%), Oklahoma (1%) and Oregon (2%) — reported a higher share of deaths in long-term care facilities in April compared with December.
But eight states experienced an increase in coronavirus cases in long-term care facilities between March and April. The increase ranged from 6% in New Hampshire to a more than 150% jump in Connecticut and Michigan. Other states that saw an increase in long-term care facility cases from March to April were Idaho (9%), Louisiana (31%), New Jersey (36%), Ohio (78%) and Alabama (81%).
KFF said these increases may reflect community spread, be due to increasing infections among younger people due to “pandemic fatigue,” or the rise of the B.1.1.7 variant.
No states reported increases in long-term care cases and deaths between March and April. The KFF analysis noted that “it remains to be seen” whether recent case increases in a few states will lead to increases in deaths.




