The Centers for Medicare & Medicaid Services came under withering criticism this week for allegedly failing to target fraud and waste. The latest salvos were delivered during a House subcommittee hearing, in which a top CMS leader was grilled repeatedly.
Lawmakers accused the agency of failing to take action on recommendations intended to prevent improper payments.
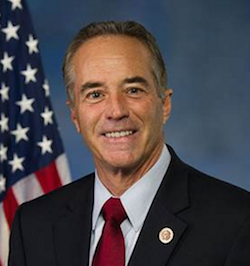
“If you worked for me, you’d be fired this afternoon,” Rep. Chris Collins (R-NY) told Shantanu Agrawal, M.D., deputy administrator and director of the CMS’ Center for Program Integrity.
The hearing coincided with the release of three Department of Health and Human Services Office of Inspector General reports. They allege that nearly $80 billion of Medicare and Medicaid payments to operators was misspent.
Agrawal, however, countered that the agency has implemented 38 Government Accountability Office and 122 OIG recommendations during the past year. He added that enhanced screening has saved Medicare $2.4 billion.
Agrawal admitted that improper Medicare and Medicaid payment rates have risen in recent years. But he attributed much of the uptick to new Affordable Care Act requirements.



