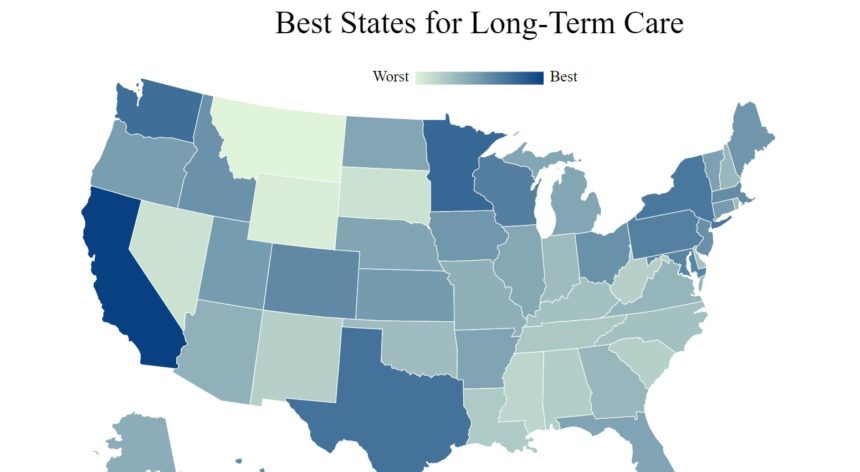
A comparison of cost, access and quality has launched California to the top of MedicareGuide’s list of top states for long-term care.
The Sunshine State topped the best lists for assisted living costs per month, adult day services total licensed capacity, homemaker services per month, and home health aide costs per month.
States rounding out the top five for long-term care are Minnesota, Washington, Texas and New York. Bottom-ranking states for older adults needing long-term care services are Montana, Wyoming, South Dakota, Nevada and Mississippi.
New York ranked as the best state for total Medicaid payments for those living with Alzheimer’s or other dementias, home health aides per capita, and Medicaid expenditures per resident.
Other ranked categories included certified geriatricians per capita — Hawaii ranked best, Montana worst; adult daycare costs per month — Texas ranked best, Washington, D.C., worst; nursing / assisted living homes per capita — Iowa ranked best, Arizona worst; nurse staffing hours per resident per day — Alaska ranked best, Illinois worst; and number of hospitalizations per 1,000 long-stay resident days — Alaska ranked best, Louisiana worst.
Under quality, California ranked best for the percentage of long stay residents whose need for help with daily activities increased. Maryland ranked worst. Hawaii led the states at best for COVID-19 death rate over 85, while Rhode Island ranked worst.
Long-term care costs can vary based on the type of care needed, timeframe, provider and location. Some of the most expensive costs include assisted living, memory care, nursing home care, home health aides and adult day healthcare services.
According to Jeff Smedsrud, co-founder and president of insurance for HealthCare.com, who provided insight for the list, the number of people needing help with activities of daily living will double from 7 million to 14 million by 2065. The Social Security Administration projects 95 million people will be 65 and older by then, and 15% of those older adults will have at least two disabilities.
The proposed Better Care Better Jobs Act would invest $400 billion into Medicaid home- and community-based services infrastructure. Senior living industry advocates are hopeful the funding will expand access to services, eliminate waitlists, address inequities and strengthen the workforce.


