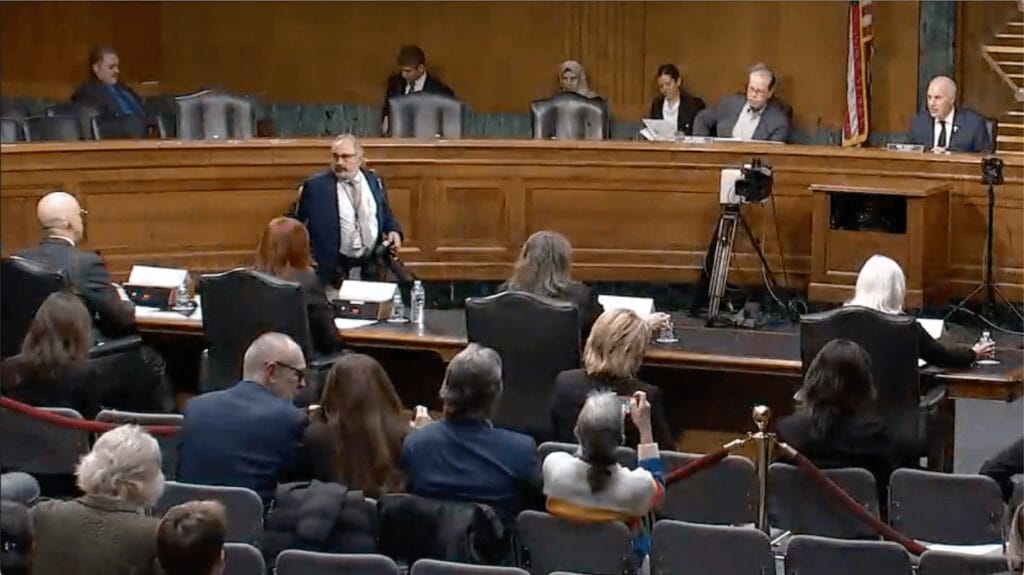
The spotlight on the assisted living industry got a little hotter on Thursday as congressional leaders called for a government study on industry pricing and transparency, announced a website and email address where consumers can share their bills and their experiences interacting with providers, and pondered increased federal involvement.
The US Senate Special Committee on Aging held its first hearing in more than 20 years that focused specifically on assisted living, which came as it awaits responses from three large operators about their efforts related to safety, staffing and pricing.
Both the hearing and the review were coordinated in response to recent articles in The Washington Post, which in December reported on the deaths of several residents with dementia who had eloped from communities, as well as November articles by the New York Times and KFF Health News, which reported on an industry pricing structure that adds fees on top of basic charges to cover additional services, as well as rate increases and the for-profit status of most providers.
Read industry reaction to the hearing: Assisted living provides value, satisfaction in long-term care continuum, industry advocates say
The committee heard testimony from and asked questions of a gerontology expert, an affordable assisted living provider, a long-term care policy analyst and a private citizen whose husband was an assisted living resident.
At the conclusion of the hearing, Casey announced that he and several Democratic colleagues had sent a letter to the Government Accountability Office asking it to study how much federal money is spent on assisted living communities, the cost of assisted living services, and the transparency and availability of that information to consumers. This move followed Casey’s letters to Brookdale Senior Living, Atria Senior Living and Sunrise Senior Living — three of the largest corporate owners and operators of assisted living communities in the country — asking for information on their workforce issues and cost structures.
Casey also called on assisted residents and their families across the country to share their stories and bills, to call out the “exorbitant cost and insidious hidden fees” charged by some operators. Alternatively, consumers can email information to [email protected].
“We have an obligation to ensure that all Americans have access to the quality care they need to age with dignity,” Casey said. “Unfortunately, what I heard today makes clear that we have a long way to go when it comes to guaranteeing the level of care that older Americans in assisted living facilities deserve. We must do better by the residents of these facilities and their families and ensure that safe and affordable care are widely available.”
‘It’s time for the federal government to step in’
It’s been more than 20 years since the Senate Special Committee on Aging held a hearing on assisted living. The Center for Excellence in Assisted Living, known as CEAL@UNC for about a year now, itself was launched in 2003 as a result of a recommendation in the landmark Assisted Living Workgroup Report delivered to the committee.
Sen. Elizabeth Warren (D-MA) addressed her tenure on the Aging Committee, including an ask with other senators in 2015 for the Government Accountability Office to report on Medicaid oversight and care quality in assisted living communities. That request resulted in a 2018 GAO report, which Warren said revealed “serious” health and safety problems in assisted living communities that have not been addressed yet.
“Assisted living facilities are governed by a patchwork of state laws without any meaningful federal oversight,” the senator said, adding her belief that it is time to require additional reporting on problems at such communities, which she said was a priority recommendation from the 2018 GAO report. “This has gone on long enough without oversight, and Congress must look at ways to improve accountability, transparency and quality of care in assisted living facilities.”
Casey said that the “dramatic” growth of assisted living in recent decades makes it long past time for Congress to re-examine the model to ensure that it is meeting the nation’s needs. The United States, he added, must have the best long-term care system in the world.
“We’re not there yet,” he said.
Ranking member Sen. Mike Braun (R-IN) pointed to his home state of Indiana, saying that it uses a combination of state and federal tools to provide more affordable assisted living options for older adults, which he said has led to improvements in affordability and quality.
“Some of my colleagues may be tempted to call for shifts in increased federal involvement and regulation. I’d say be careful,” Braun said. “Help us get best practices out there. Help us have an environment to get it done more efficiently, more affordably at lower levels of government. I believe that states are best positioned to meet that growing need.”
But operators, he said, should support transparency and data-sharing.
Witness Richard Mollott, executive director of the New York City-based Long Term Care Community Coalition, said that three developments over the past 40 years have “drastically” changed the nature and character of the assisted living sector: a dramatic increase in resident needs and frailty, a significant increase in private payment for and government interest in assisted living, and the adoption of increasingly sophisticated and large-scale corporate models by operators, including ownership by real estate investment trusts, private equity and other private investment structures.
At the same time, he said, the “typical” assisted living resident has grown older, has more chronic health conditions and is more likely to have a cognitive impairment diagnosis. The business model of assisted living, Mollot added, leads many communities to accept residents for whom they are unable to provide safe and dignified care, leaving families and residents vulnerable to fraud.
“Too many seniors and families get taken in by promises of ‘memory care’ and aging in place, when in fact, these are more often marketing terms than accurate representations of specialized care,” Mollot said. “The absence of any federal quality or safety standards, coupled with the virtual absence of any reliable information of the quality, safety and cost of assisted living, have made assisted living a sector ripe for investment by sophisticated private enterprises who can shuffle around resources and take profits with little regard for the promises made to seniors and their families.”
Pointing to the “growing chorus” of local and national news reports alleging neglect, “disastrous elopements” and “financial shenanigans” occurring within the assisted living sector, Mollot said that it is clear that the industry has reached the “crisis point” that nursing homes reached 40 years ago, which led to congressional action.
He recommended establishing national standards to promote quality, safety and integrity in assisted living, as well as a national database with information and metrics to evaluate cost and quality. Mollot also promoted resident and family engagement to help ensure that assisted living is truly a home- and community-based service.
“I think it’s time for the federal government to step in,” he said. “The same population, in terms of the number of people, are in assisted living as are in nursing homes, but we don’t know what’s happening to them. We don’t know the care they’re receiving.”
States “are just not inclined to take action,” he added.
“It really is time for the federal government to step in to ensure that wherever someone accesses dementia care, that means something,” Mollot said.
Supporting the direct care workforce
Witness Jennifer Craft Morgan, PhD, director of the Gerontology Institute at Georgia State University, said that person-centered dementia care is necessary to support an individual’s preferences, communication style, care and support needs.
Approximately 42% of assisted living residents have a dementia diagnosis, but Morgan said that the disease is underreported because many older adults are not screened or tested despite showing symptoms related to their memory and thinking. Regardless, many of the aides and direct care workers who care for residents living with dementia are paid an hourly wage of $15 and do not receive dementia-specific training, she said.
“The system we’ve set up works against them,” Morgan said. “Direct care workers in long-term care settings experience low wages, few benefits, heavy workloads, dangerous jobs and little no career mobility.”
Long-term care that is person-centered, community-minded and empowering for residents, staff members and care partners has a much better chance of success, Morgan said. She recommended improving and standardizing initial and continuing education training for direct care workers and staff members, professionalizing the direct care workforce, incentivizing and rewarding good employers who deliver high-quality care, increasing access to assisted living, improving care coordination and resources for people living with dementia and their “care partners,” and supporting standardization of monitoring and resources to increase state-based oversight and transparency.
Making care affordable
Witness Julie Simpkins, co-president of Indianapolis-based Gardant Management Solutions and an at-large member of the National Center for Assisted Living Board of Directors, described her company’s “unique model” of providing affordable assisted living to low-income older adults through Medicaid home- and community-based waivers.
She said that Gardant is the fifth largest assisted living provider in the country and the largest in Indiana, although it was unclear what that national standing was based on. Gardant ranked 27th on the 2023 Argentum largest provider list and 32nd on the 2023 ASHA 50 list of operators.
Simpkins said that Gardant is limited in where it can offer its services due to the variability of state Medicaid waiver programs, state reimbursement levels and the number of available waiver spots. Public-private partnerships are necessary to incentivize more providers to develop models to care for this population, she said.
“It is critical that policies and regulations help protect residents while still supporting their freedom of movement and independence,” Simpkins said. “Assisted living is a critical aspect of the long-term care continuum and dedicated to delivering person-centered care to our nation’s seniors.”
Expanding more affordable long-term care options and addressing caregiver shortages through workforce programs could make a difference, she said.
The hearing is available for viewing on the Aging Committee’s website along with the prepared remarks of Casey, Braun and the hearing witnesses.